High Fat Ketogenic Diet & Brain Cancer by Dr. Luminita Alexe, ND
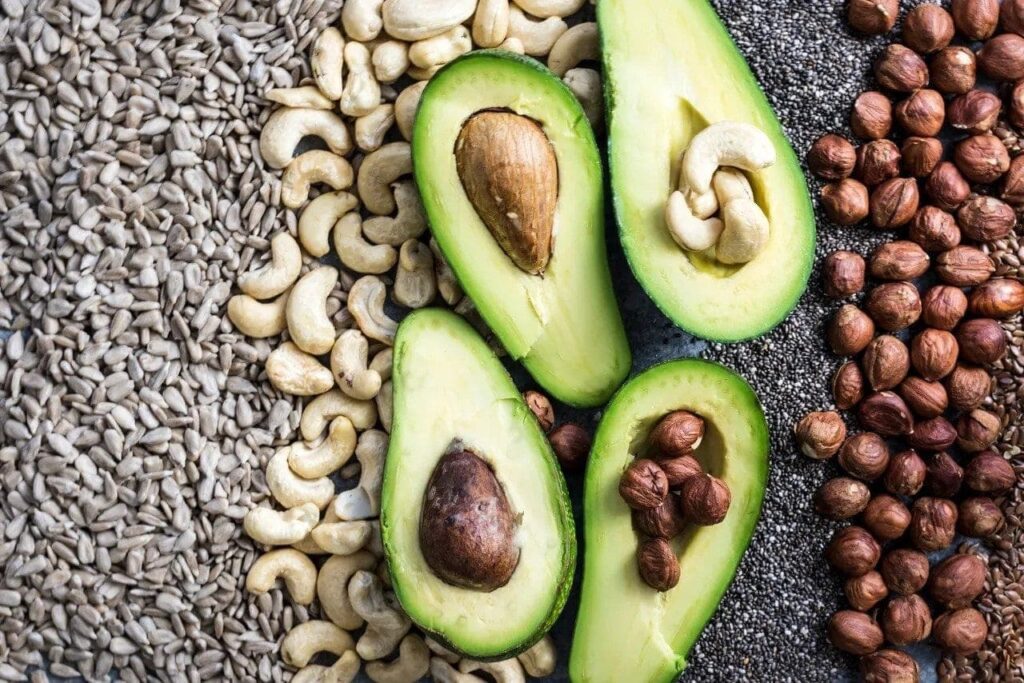
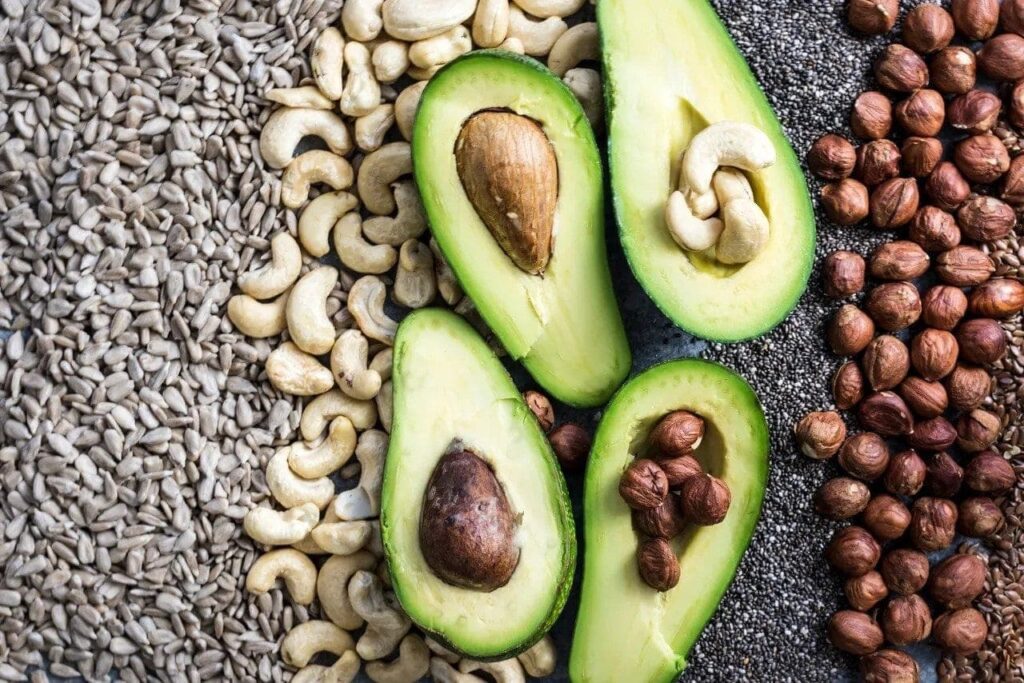
High Fat Ketogenic Diet & Brain Cancer – Many of us have heard of the high fat, ketone inducing Ketogenic Diet, and its effect on weight loss. A high fat, bacon laden diet may seem like a dream come true to many. And, research suggests this diet may just have some unintended positive health consequences other than weight loss: cancer management.
Let’s take a look at Glioblastoma multiforme (GBM) as it is the most common malignant primary brain tumor in adults and generally considered to be universally fatal. GBM accounts for 12-15% of all intracranial neoplasms and affects 2 to 3 adults per 100,000 annually. Mean survival rate in adults of 12-18 months with standard therapy and 3 to 6 months without therapy.
A Metabolic Disease
Due to it being a primary metabolic disease, malignant brain cancer can be managed through changes in the metabolic environment. In contrast to normal neurons and glia, which readily transition to ketone bodies (∆-hydroxybutyrate) for energy under reduced glucose, malignant brain tumors are strongly dependent on glycolysis for energy. It is believed that this was an evolutionary adaptation in times of food deprivation that allowed for the survival of normal cells. Only cells with normal mitochondria and genome can effectively transition from one energy state to another. Mutations restrict genomic and metabolic flexibility thus making tumor cells more vulnerable to energy stress than a normal cell.
Little progress has been made in the long-term management of glioblastoma multiforme (GBE), which is the most aggressive and lethal of brain cancers. Glucose and glutamine are major fuels for myeloid cells as well as rapidly dividing cancer stem cells. Metabolic therapy is designed to target what is metabolically common to all tumor cells (aerobic fermentation). Current therapies that increase inflammation and energy metabolites in GBM can accelerate tumor progression. The calorie-restricted ketogenic diet has been shown to reduce fermentable fuels in the tumor microenvironment and exhibit anti-angiogenic, anti-inflammatory, and pro-apoptotic properties.
Glucose Reliance on Tumor Cells
Tumor cells have an increased reliance on glucose, indicating the therapies affecting cellular metabolism may be an effective way to improve current therapies. A ketogenic diet and calorie restriction can cause a lowering of blood glucose and an increase in blood ketones, thus causing a metabolic change. Some data suggest that low blood glucose levels during the treatment of glioblastoma may improve outcomes. In one analysis of 53 patients, 6 underwent a ketogenic diet during treatment, and of those 4 were alive at a median follow-up of 14 months.
Mitochondrial Enzyme Defect
One study of brain biopsies investigated the expression of several key enzymes involved in ketolytic and glycolytic metabolism in human anaplastic glioma and glioblastoma. The results showed that malignant gliomas have different expressions of ketolytic and glycolytic enzymes. The rate-limiting mitochondrial ketolytic enzymes (OXCT1 and BDH1) were either low or very low in 14 of the 17 glioblastomas. It was hypothesized that patients with low expression of ketolytic enzymes in their malignant gliomas may respond better to ketogenic diets than those with positive expression of these enzymes. Recent animal models suggest that glioma cells are more dependent on glycolysis for energy generation showing therapeutic results using a ketogenic diet. Ketogenic diet effectively appears to starve the glioma cell while providing ketone bodies as an energy source for normal neurons and glial cells.
The Warburg Effect
The differential in the utilization of ketone bodies by neurons and glioma cell lines was observed. Even in the presence of oxygen, malignant cells often highly depend on glycolysis for energy generation, a phenomenon known as the Warburg effect. In oncology, the Warburg effect is the observation that most cancer cells predominantly produce energy by a high rate of glycolysis followed by lactic acid fermentation in the cytosol, rather than by a comparatively low rate of glycolysis followed by oxidation of pyruvate in mitochondria as in most normal cells. The latter process is aerobic (uses oxygen). Malignant, rapidly growing tumor cells typically have glycolytic rates up to 200 times higher than those of their normal tissues of origin; this occurs even if oxygen is plentiful.
Hyperbaric Oxygen Treatment
Ketogenic diet alone significantly decreased blood glucose, slowed tumor growth, and increased mean survival time by 56.7% in mice with systemic metastatic cancer. Combining the ketogenic diet with hyperbaric oxygen therapy elicited a decrease in blood glucose, tumor growth rate, and a 77.9% increase in mean survival times compared to controls. Evidence shows that these therapies when combined produced a significant anti-cancer effect and should be further investigated as potential non-toxic treatments or adjuvant therapies to standard care.
Calorie Restriction
Calorie restriction was also shown to be effective at reducing malignant brain tumor growth and invasion. An innovative brain cancer model was developed in an inbred mouse strain that shares characteristics with human glioblastoma multiforme. The efficacy of calorie restriction for its ability to reduce tumor size and invasion was measured using bioluminescence imagining. Calorie restriction significantly reduced the invasion of tumor cells from the implanted ipsilateral hemisphere into the contralateral hemisphere.
There is an opinion that the failure to recognize brain cancer as a disease of energy metabolism has contributed in large part to the failure in management and that as long as the brain tumors have access to glucose and glutamine, the disease will progress. The current standard of care allows for access to glucose and glutamine. A ketogenic diet targets major signaling pathways associated with glucose and glutamine metabolism and is anti-angiogenic, anti-inflammatory, and pro-apoptotic in rodent models. It would be worth discussing with your oncologist if adding a ketogenic diet may be of therapeutic benefit.
**Disclaimer**
This site and its services are for consumer educational use only. Nothing contained in this article is or should be considered or used as a substitute for medical advice, diagnosis, or treatment. Never start any diet, exercise, or supplement program without consulting your medical provider. This article and its services do not constitute the practice of medicine. Users should always seek the advice of a physician with any questions regarding their health or medical conditions. Never disregard, avoid, or delay obtaining medical advice or following the advice of a physician because of something you have seen or read on this site.
References:
1)Seyfried TN, Flores R, Poff AM, D’Agostino DP, Mukherjee P. Metabolic therapy: A new paradigm for managing malignant brain cancer. Cancer Lett. 2014 Jul 25. pii: S0304-3835(14)00352-8. DOI: 10.1016/j.canlet.2014.07.015. [Epub ahead of print] PubMed PMID: 25069036.
2)Rieger J, Bähr O, Maurer GD, Hattingen E, Franz K, Brucker D, Walenta S, Kämmerer U, Coy JF, Weller M, Steinbach JP. ERGO: a pilot study of ketogenic diet in recurrent glioblastoma. Int J Oncol. 2014 Jun;44(6):1843-52. doi: 10.3892/ijo.2014.2382. Epub 2014 Apr 11. PubMed PMID: 24728273; PubMed Central PMCID: PMC4063533.
3)Champ CE, Palmer JD, Volek JS, Werner-Wasik M, Andrews DW, Evans JJ, Glass J, Kim L, Shi W. Targeting metabolism with a ketogenic diet during the treatment of glioblastoma multiforme. J Neurooncol. 2014 Mar;117(1):125-31. DOI: 10.1007/s11060-014-1362-0. Epub 2014 Jan 19. PubMed PMID: 24442482.
4)Woolf EC, Scheck AC. The Ketogenic Diet for the Treatment of Malignant Glioma. J Lipid Res. 2014 Feb 6. [Epub ahead of print] PubMed PMID: 24503133.
5)Paoli A, Rubini A, Volek JS, Grimaldi KA. Beyond weight loss: a review of the therapeutic uses of very-low-carbohydrate (ketogenic) diets. Eur J Clin Nutr. 2013 Aug;67(8):789-96. DOI: 10.1038/ejcn.2013.116. Epub 2013 Jun 26. Review. Erratum in: Eur J Clin Nutr. 2014 May;68(5):641. PubMed PMID: 23801097; PubMed CentralPMCID: PMC3826507.
6)Maroon J, Bost J, Amos A, Zuccoli G. Restricted calorie ketogenic diet for the treatment of glioblastoma multiforme. J Child Neurol. 2013 Aug;28(8):1002-8. DOI: 10.1177/0883073813488670. Epub 2013 May 13. Review. PubMed PMID: 23670248.
7)Chang HT, Olson LK, Schwartz KA. Ketolytic and glycolytic enzymatic expression profiles in malignant gliomas: implication for ketogenic diet therapy. Nutr Metab (Lond). 2013 Jul 5;10(1):47. DOI: 10.1186/1743-7075-10-47. PubMed PMID: 23829383; PubMed Central PMCID: PMC3707813.
8)Caso J, Masko EM, Ii JA, Poulton SH, Dewhirst M, Pizzo SV, Freedland SJ. The effect of carbohydrate restriction on prostate cancer tumor growth in a castrate mouse xenograft model. Prostate. 2013 Apr;73(5):449-54. DOI: 10.1002/pros.22586. Epub 2012 Oct 4.PubMed PMID: 23038057; PubMed Central PMCID: PMC3594433.
9)Martinez-Outschoorn UE, Lin Z, Whitaker-Menezes D, Howell, Sotgia F, Lisanti MP.Ketone body utilization drives tumor growth and metastasis. Cell Cycle. 2012 Nov1;11(21):3964-71. DOI: 10.4161/cc.22137. Epub 2012 Sep 19. PubMed PMID: 23082722;PubMed Central PMCID: PMC3507492.
10)Seyfried TN, Marsh J, Shelton LM, Huysentruyt LC, Mukherjee P.Is the restricted ketogenic diet a viable alternative to the standard of care for managing malignant brain cancer? Epilepsy Res. 2012 Jul;100(3):310-26. DOI: 10.1016/j.eplepsyres.2011.06.017.Epub 2011 Aug 31. Review. PubMed PMID: 21885251.
11)Klement RJ, Kämmerer U. Is there a role for carbohydrate restriction in the treatment and prevention of cancer? Nutr Metab (Lond). 2011 Oct 26;8:75. DOI: 10.1186/1743-7075-8-75. PubMed PMID: 22029671; PubMed Central PMCID: PMC3267662.
12)Eloqayli H, Melø TM, Haukvik A, Sonnewald U.[2,4-(13)C]β-hydroxybutyratemetabolism in astrocytes and C6 glioblastoma cells. Neurochem Res. 2011Aug;36(8):1566-73. DOI: 10.1007/s11064-011-0485-3. Epub 2011 May 3. PubMedPMID: 21538079; PubMed Central PMCID: PMC3139091.
13)Schmidt M, Pfetzer N, Schwab M, Strauss I, Kämmerer U.Effects of a ketogenic diet on the quality of life in 16 patients with advanced cancer: A pilot trial. Nutr Metab (Lond).2011 Jul 27;8(1):54. DOI: 10.1186/1743-7075-8-54. PubMed PMID: 21794124; PubMedCentral PMCID: PMC3157418.
14)Maurer GD, Brucker DP, Bähr O, Harter PN, Hattingen E, Walenta S, Mueller-KlieserW, Steinbach JP, Rieger J.Differential utilization of ketone bodies by neurons and glioma cell lines: a rationale for the ketogenic diet as experimental glioma therapy. BMCCancer. 2011 Jul 26;11:315. DOI: 10.1186/1471-2407-11-315. PubMed PMID: 21791085;PubMed Central PMCID: PMC3199865.
15)Seyfried TN, Kiebish MA, Marsh J, Shelton LM, Huysentruyt LC, Mukherjee P.Metabolic management of brain cancer. Biochim Biophys Acta. 2011 Jun;1807(6):577-94. DOI: 10.1016/j.bbabio.2010.08.009. Epub 2010 Sep 8. Review. PubMed PMID:20804725.
16)Shelton LM, Huysentruyt LC, Mukherjee P, Seyfried TN.Calorie restriction as an anti-invasive therapy for malignant brain cancer. ASN Neuro. 2010 Jul 23;2(3):e00038. DOI: 10.1042/AN20100002. PubMed PMID: 20664705; PubMed Central PMCID: PMC2908744
17)Poff AM, Ari C, Seyfried TN, D’Agostino DP. The ketogenic diet and hyperbaric oxygen therapy prolong survival in mice with systemic metastatic cancer. PLoS One. 2013 Jun 5;8(6):e65522. DOI: 10.1371/journal.pone.0065522. Print in 2013. PubMed PMID: 23755243; PubMed Central PMCID: PMC3673985.
18)Maurer GD, Brucker DP, Bähr O, Harter PN, Hattingen E, Walenta S, Mueller-Kleiser W, Steinbach JP, Rieger J. Differential utilization of ketone bodies by neurons and glioma cell lines: a rationale for the ketogenic diet as experimental glioma therapy. BMC Cancer. 2011 Jul 26;11:315. DOI: 10.1186/1471-2407-11-315. PubMed PMID: 21791085; PubMed Central PMCID: PMC3199865
***DISCLAIMER
The information provided on this Site is for educational purposes only. Please consult a physician before beginning any treatment program or making any adjustments in your healthcare, diet, and /or lifestyle. Do not remove yourself from any prescribed medications or treatments without consulting your doctor. Any and all dietary supplements or nutritional products discussed on this Site are not FDA-approved and are not intended to diagnose, treat, prevent, or cure any disease.
