Amylin: Effects, Uses, and Exciting Research

Amylin, or islet amyloid polypeptide (IAPP) plays an important role in glycemic regulation. It helps you feel satiated and slows gastric emptying. Irregular levels of amylin can affect both Type 1 and Type 2 diabetes. Amylin and its co-secretion insulin are instrumental in controlling blood glucose, as well as appetite and weight. This article will provide an overview of how amylin works, the roles it plays, and how we use its analog, pramlintide, to aid in regaining balance.
What is Amylin?
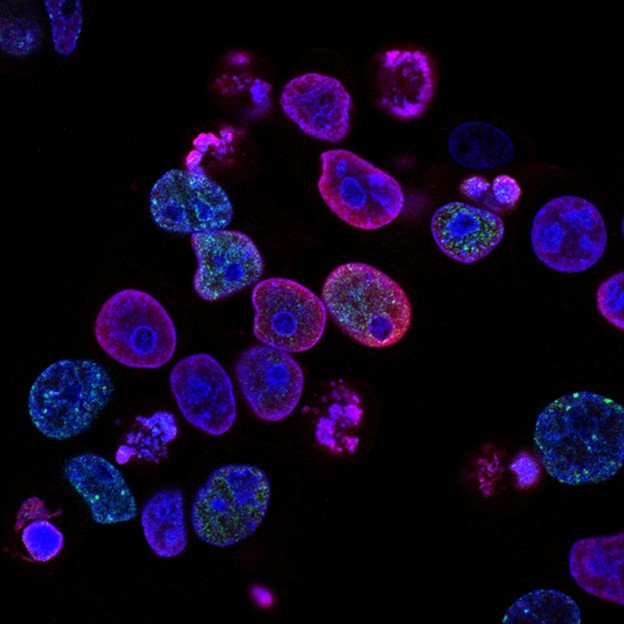
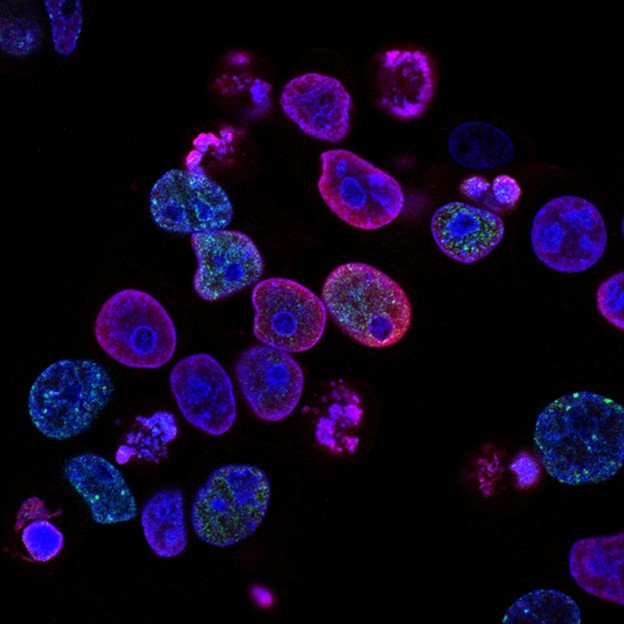
Amylin is a peptide made up of 37 amino acids – the building blocks of the body. Amylin is secreted by the pancreatic beta-cells, which also secrete insulin at the same time, in response to nutrient intake. This secretion is released in a ratio of 100 to 1 (insulin to amylin). Amylin and insulin work together to regulate nutrient levels in the blood.
Amylin, also called islet amyloid polypeptide (IAPP), is a 37-amino acid peptide hormone co-secreted with insulin by the pancreatic β cells. This happens in response to food intake, with insulin and amylin released in a ratio of about 100:1. Together, they play crucial roles in glucose homeostasis, regulating blood sugar levels, appetite, and weight.pen_spark
Amylin promotes the feeling of satiety by slowing gastric emptying. It also prevents spikes in blood glucose levels after meals. Altogether, these effects help regulate the blood sugar, which is important for normal bodily function. When blood sugar levels are outside of the normal range, it can indicate a medical condition, like diabetes.
Amylin’s Origins and Variations
- Pancreatic Islets: The Source: Remember, amylin gets its alternate name, islet amyloid polypeptide, because it’s produced within specialized clusters of cells called pancreatic islets. These contain the insulin-producing beta cells, where amylin is also created and stored.
- Species Differences: Rat vs. Human Amylin: Interestingly, rat amylin differs in its amino acid residues compared to human islet amyloid polypeptide (hIAPP). This difference is why rat amylin doesn’t form the problematic amyloid fibrils, making it a valuable tool in research, though not for direct human treatment.
Amylin in Diabetes Management
- Exogenous Amylin: A Therapeutic Avenue: The use of pramlintide demonstrates the concept of replacing deficient hormones with exogenous (externally sourced) ones. This approach is already well-established with insulin therapy in diabetes mellitus and could expand as science learns more about amylin’s actions.pen_spark
How Does Amylin Affect the Body?
When amylin is out of balance, we primarily see issues with diabetes. People with Type 1 diabetes are deficient in amylin, while people in the early stages of Type 2 diabetes have elevated levels of the peptide. It’s worth noting, too, that Type 2 diabetes is characterized by hyperinsulinemia – elevated levels of insulin. However, as time goes on, people in the later stages of Type 2 diabetes experience deficiencies in amylin secretion.
Partnership with Insulin: Amylin complements insulin’s actions. While insulin focuses on storing glucose, amylin slows gastric emptying, promotes satiety (feeling full), and suppresses glucagon secretion (a hormone that raises blood sugar). This combined effect prevents spikes in blood sugar after meals.
Diabetes Connection: Imbalances in amylin are closely linked to diabetes. Type 1 diabetes is characterized by amylin deficiency, while early-stage Type 2 diabetes often shows elevated amylin levels. However, later-stage Type 2 diabetes may involve impaired amylin secretion.
Beyond Blood Sugar: Research suggests amylin might influence other conditions. Elevated levels are seen in individuals with obesity, impaired glucose tolerance, and even during pregnancy.
Amylin and the Brain: Studies point to a potential link between amylin and neurodegenerative diseases like Alzheimer’s. Both amylin and beta-amyloid (a hallmark of Alzheimer’s) can form amyloid plaques. Early stages of central nervous system (CNS) amyloid build-up might be linked to high amylin states, while later stages may relate to low amylin levels.
Although early research seemed to show that amylin inhibits insulin secretion leading to insulin resistance and the development of Type 2 diabetes, a body of more recent research suggests otherwise. We now know that amylin is an active pancreatic islet hormone – it works alongside insulin and glucagon to maintain glucose balance. Since amylin influences gastric emptying, it regulates the rate at which glucose flows into circulation. As a result, amylin controls how quickly glucose from our meals enters our systems and limits its release as well as hepatic glucose production. In all, it’s clear that amylin works with insulin to control blood sugar.
It’s also worth noting that we sometimes see increased levels of amylin in the plasma outside of people with diabetes. This includes people with obesity and those with impaired glucose tolerance. Pregnant women with normal glucose tolerance and those with gestational diabetes also sometimes have higher levels of plasma amylin.
Additionally, epidemiological studies have shown a clear link between metabolic disorders and neurodegenerative disorders. In particular, these studies have established a connection between Type 2 diabetes and Alzheimer’s disease. With this in mind, researchers believe that amylin could have a key role in acting as the interface between these two types of disorders.
Uses for Amylin

In theory, amylin replacement could help improve glycemic control for diabetic people. Unfortunately, human amylin has certain properties that make it cluster and form amyloid fibers that may cause the destruction of beta cells in Type 2 diabetes. Since we need beta cells to make insulin, using amylin as a medication would be harmful.
Instead, scientists have developed a stable analog – pramlintide. Pramlintide has similar pharmacokinetic and pharmacodynamic properties to amylin, as well as similar actions. About 5,000 patients have been treated with pramlintide across a number of clinical trials. Thanks to these tests, we know that pramlintide is both safe and effective.
Further research is needed to understand whether adjusting amylin levels could aid in treating Alzheimer’s disease. Researchers do know that both amylin and beta-amyloids are prone to forming amyloid plaque and cytotoxic effects. Amylin can form these plaques in pancreatic islet cells as well as the central nervous system (CNS). In the CNS, it can co-localize with beta-amyloid plaques in some Alzheimer’s disease patients. With this knowledge, researchers theorize that amylin could be a second amyloid in neurodegenerative disorders.
Additionally, we may be able to learn something from where and when these plaques form. There’s some evidence that early processes of amyloid formation in the CNS could be related to hyperamylasemia conditions. Meanwhile, late stages of central amyloid pathologies are likely related to hypoamylinemic conditions. In short, we need to study and learn more about these relationships to potentially establish amylin-based treatment interventions. These advancements could aid in treatments for neurodegenerative disorders, as well as their metabolic comorbidities.
Understanding Amylin’s Structure
- Amino Acid Building Blocks: Amylin’s unique amino acid sequence gives it both beneficial and challenging properties. Its tendency to aggregate into amyloid fibrils is a concern in type 2 diabetes, as these fibrils can contribute to the destruction of pancreatic beta cells.
- Amylin vs. Calcitonin Gene-Related Peptide (CGRP): Amylin shares structural similarities with CGRP, a peptide involved in pain transmission and vasodilation.
Therapeutic Potential: Amylin Analogues
- The Challenge of Human Amylin: Unfortunately, human islet amyloid polypeptide (hIAPP) is not directly usable in diabetes treatment due to its tendency to form harmful amyloid plaques.
- Pramlintide: A Stable Alternative: Researchers developed pramlintide, an amylin analogue with similar effects but greater stability. Clinical trials demonstrate its safety and efficacy in improving blood glucose control when used alongside insulin therapy.
- Beyond Diabetes: Exploring Amylin’s Role in the Brain: The potential connection between amylin and neurodegeneration is an active research area. Could therapies targeting amylin help manage diseases like Alzheimer’s alongside their metabolic conditions?
The Takeaway
Amylin is a fascinating peptide, integral to healthy blood sugar regulation. For people with diabetes, understanding its intricacies is vital. Pramlintide, as an amylin replacement, adds a valuable tool alongside insulin therapy. Future research may unlock amylin’s secrets in combating a wider range of conditions, potentially including neurodegenerative diseases.
Ultimately, amylin is a key peptide that helps maintain a healthy appetite and normal blood sugar in the average person. People with diabetes have an imbalance in insulin as well as amylin. Though more research is needed, amylin and its analog could potentially aid in treating multiple conditions.
Be sure to work with your primary care physician before using this medication or schedule a consultation with one of our health consultants.
KIYA Longevity provides innovative best-in-class peptide products that meet the highest standards for safety and purity at a fraction of the cost.CerebroPep PEPTIDE (1ST NEURO
PEPTIDE)BPC-157 PURE PEPTIDE (IMMEDIATE
RELEASE)BPC-157 PURE Oral Spray (RAPID
ABSORPTION)KPV PEPTIDE (RAPID ABSORPTION)TB4-FRAG MAX PEPTIDE (HEALING AND
RECOVERY)THYMOGEN ALPHA-1 (IMMUNE SUPPTORT)Weight Loss Peptide “Can’t Weight”
Questions about other peptides? Check out Kiya Longevity’s Peptide Guide.
Resources:
https://www.sciencedirect.com/topics/neuroscience/amylin
https://www.uptodate.com/contents/amylin-analogs-for-the-treatment-of-diabetes-mellitus#H1
https://pubmed.ncbi.nlm.nih.gov/9212323/
https://www.frontiersin.org/articles/10.3389/fnins.2015.00216/full
